
In-vitro fertilisation (IVF)
IVF gives many infertile couples the best chance of achieving fertilisation and pregnancy. IVF is used for couples with tubal infertility, severe male factor infertility (where the eggs are inseminated by ICSI) and for couples with unexplained infertility
What does IVF involve?
An IVF treatment cycle involves several steps:
Ovarian stimulation
Hormonal medications are used to stimulate the ovaries to grow several follicles. These medications are usually via subcutaneous injection. You will be shown when and how to take these. You will have several blood tests and ultrasound scans to monitor your response to stimulation.
Egg collection
When the growing ovarian follicles reach the appropriate size, eggs (oocytes) can be collected from them. This is a day stay procedure that is usually performed under a deep intravenous sedation administered by an anaesthetist. A vaginal ultrasound probe is used with a needle that is guided through the top of the vagina and into the ovary. The egg collection is carried out by removing the fluid from the follicles in the ovaries and searching for the eggs in this fluid. The procedure usually takes 15-45 minutes.
Embryology
Once the eggs have been collected, sperm are then added. The following morning the eggs are assessed for fertilisation. Embryos are then cultured for up to six days.
Embryo transfer
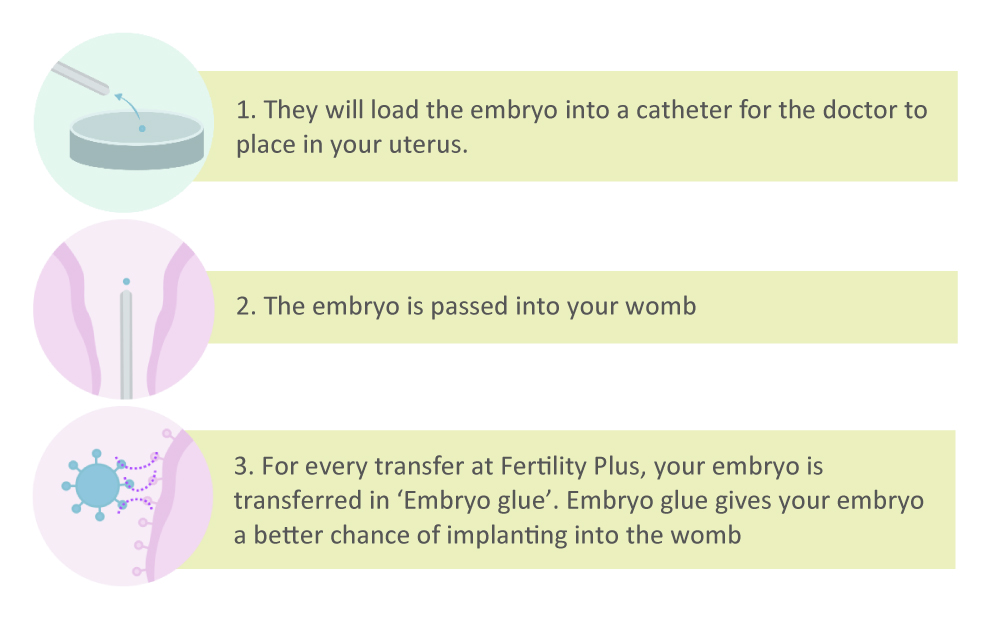
An embryo is transferred back into the uterus under ultrasound guidance three to five days following the egg collection, using a simple and gentle technique. Any remaining good quality embryos are then frozen for your future use.
Luteal phase
Medications are taken to prepare and maintain the uterine lining, to allow an embryo to implant and develop.
There are several different IVF treatment protocols available. Your doctor will tailor your treatment specifically to you.
Before starting IVF treatment, you will be invited to attend an orientation session. The orientation appointment is an opportunity for you to gain an understanding of the processes involved in fertility treatment. If you are accessing fertility treatment as a couple, it is essential that you both attend this appointment.
IVF is available both publicly and privately. Your doctor will check and advise your eligibility for publicly funded treatment. An individualised quote can be provided to you for private treatment.
Side Effects and Risks Associated With IVF Treatment
Most people tolerate treatment very well, with few side effects.
The most common side effects of the medications used in the stimulation phase of IVF are nausea, headaches and fatigue. Breast tenderness, hot flushes and dry skin may also be experienced.
As the ovaries grow and respond to treatment, some tenderness and swelling of the pelvis/abdomen may occur.
These side effects are temporary and stop on completion of treatment.
Occasionally, too many follicles develop and a condition called Ovarian Hyper Stimulation Syndrome may occur. We monitor for this closely and will advise you on management if you are at risk of this.
Your safety is our priority. We are happy to address any specific concerns you may have prior to and during your IVF cycle
What happens in the lab?
Embryologists are specially trained scientists who care for and look after your sperm, eggs and embryos. Embryologists are Healthcare Professionals registered with the Medical Sciences Council of New Zealand.
Stage 1: Egg and sperm collection
Getting Ready
Leading up to treatment, we encourage healthy lifestyles for both men and women. Eat lots of healthy food, and limit alcohol and caffeine (1 cup of coffee a day is fine). You must be smoke and drug free.
As you get closer to egg collection day, it’s helpful for partners who will be providing a fresh sample of sperm on the day to have frequent ejaculations (about every 2-3 days).
Egg collection
On the day of egg collection, after being checked in by the nurse, you will meet an embryologist. One of us will be in theatre with you to look for your eggs under the microscope as the doctor drains the fluid from the follicles on the ovaries (aspiration).
You will be told how many eggs were collected following your procedure.
Sperm collection
While you are having your egg collection, your partner needs to produce a semen sample, if using fresh sperm. We have a private room available with Wi-Fi.
-
- You must bring photo ID. This can be a driver’s license or passport
-
- Remember you must be 2-3 days without sex or ejaculation
Your embryologist will speak to you before you go home about the semen sample and confirm if your treatment will be IVF or ICSI.
If you are anxious about producing a sample at the clinic, please phone the lab (before the egg collection day) to talk about back up sperm freezing or bringing the sample from home.
Insemination
Insemination happens around four hours after your eggs have been collected.
We will add sperm to your eggs by standard insemination (IVF) if your sperm has ‘washed’ up well. Washing the sperm is a process where we separate the dead and immotile sperm from the strong, motile sperm.
With standard insemination, we add a large number of motile sperm to the dish with your eggs. Overnight, sperm swim to the eggs. Approximately 60-80% of eggs should fertilise in the presence of sperm.
If your doctor has recommended Intracytoplasmic Sperm Injection (ICSI) for male factor infertility, we will inject all the mature eggs. On average, 80% of eggs are expected to be mature.
A single sperm is carefully injected into each mature egg. Sometimes, the eggs do not survive the injection and this can happen up to 5% of the time.
Stage 2: Embryo growth
Day 1 after egg collection
Fertilisation Your embryo is one day old! Your embryologist will check your eggs for fertilisation. Usually, 60-80% of eggs fertilise. Results Your embryologist will phone you in the morning (the day after egg collection) with your fertilisation results. Very occasionally, failed fertilisation occurs. This is when no eggs have fertilised. This happens in around 1-3% of cycles. A nurse will call you in the afternoon to check how you are and give you a provisional transfer time on day 3.
Day 3 after egg collection

Your embryologist will phone you in the morning to confirm whether your transfer will go ahead today (day 3) or wait an extra 2 days (day 5). This decision is based on how the embryo develops over the last 3 days. Embryo transfer If the transfer goes ahead on this day, your embryologist will select your best embryo for transfer.
-
- Transfers are similar to having a smear test done.
-
- You will need a full bladder for this procedure.
-
- Embryo transfers do not involve sedation so you are able to eat normally.
Day 5-6

After your embryo transfer, whether on day 3 or day 5, any leftover embryos will be assessed for freezing at the blastocyst stage (day 5-6).
On average about 30% of fertilised eggs form blastocysts. In some couples, we see much higher than this and in some couples no blastocysts develop. 50% of our couples have embryos suitable for freezing.
Your embryologist will call you on the afternoon of day 6 to let you know if your embryos were suitable for freezing. Your embryologist will email you a lab summary of your cycle after day 6.
Treatment Add-ons
These are the adjuvant therapies that Fertility Plus currently offers. Please speak to your doctor if you would like more information on the effectiveness, the risks and the cost of each Add-On. Please note that at Fertility Plus we transfer every embryo in Embryo Glue.
Add-ons include:
-
- Pre-implantation Genetic Testing for Aneuploidy (PGT-A)
-
- Artificial Egg Activation
-
- DHEA
-
- Testosterone
-
- CoQ10
-
- hCG Infusions
Single embryo transfer (SET)
Fertility Plus has a policy of single embryo transfer. The principle of single embryo transfer is to give each single embryo that is transferred its maximum opportunity to implant and develop into a healthy pregnancy, as well as prevent ‘avoidable’ multiple pregnancies.
Twin pregnancies carry a much greater risk for pregnant women and for the foetuses/babies than singleton pregnancies.




